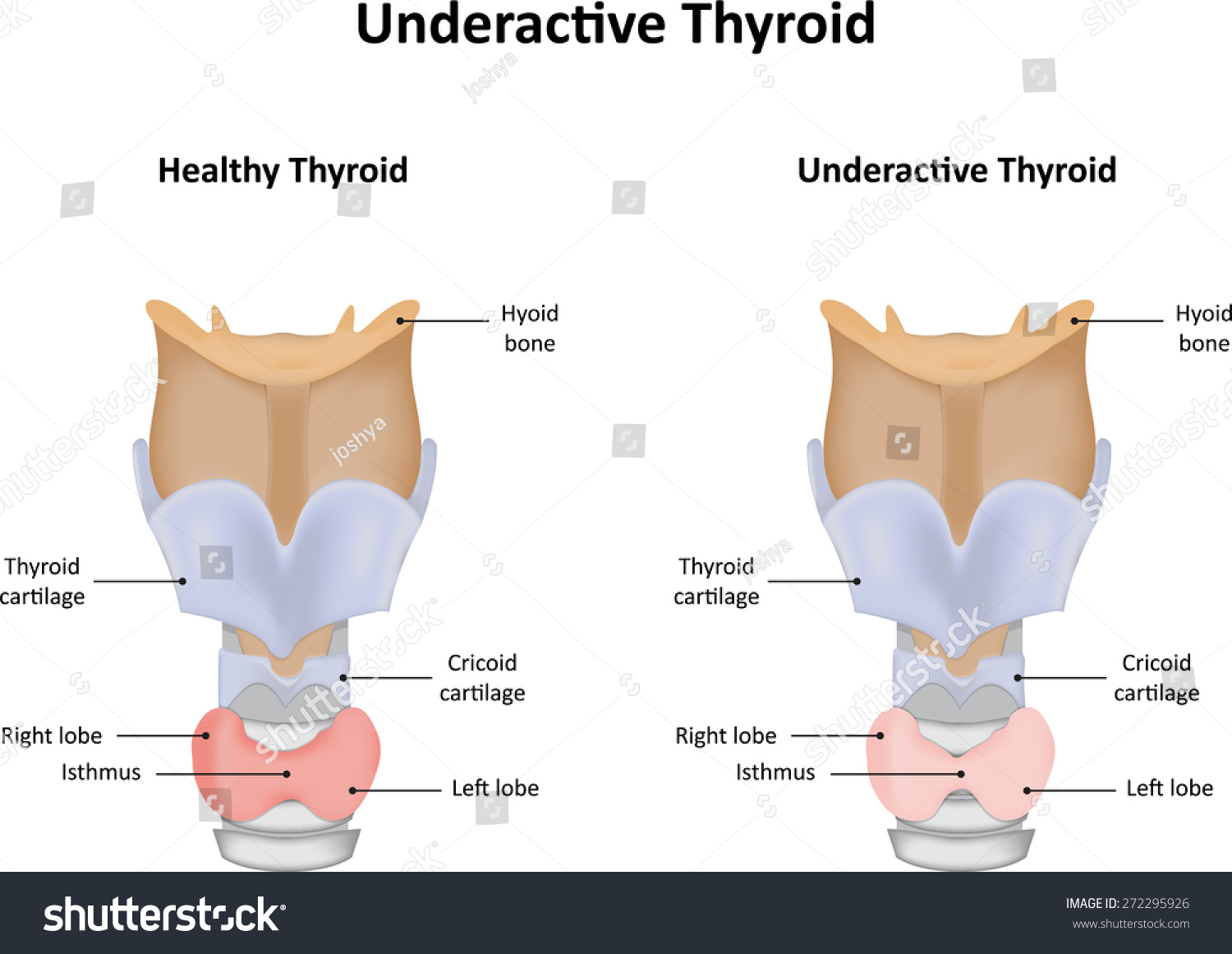
An underactive thyroid gland, also known as hypothyroidism, is a medical condition that occurs when your thyroid gland does not produce enough hormones. Located in the front lower part of the neck below the larynx, the thyroid gland is made up of special cells that produce hormones. Hormones are chemical messengers in your body that send information to the organs and tissues, controlling processes such as mood, growth, and metabolism. Your thyroid produces two thyroid hormones (triiodothyronine and thyroxine) that regulate the way your body uses energy from food or your body’s metabolism. Your metabolism is an important factor that affects your heartbeat, your body’s temperature, and how well you burn calories, among other things. When you don’t have enough thyroid hormones, the process in your body slows down. As a result, your body makes less energy and your metabolism becomes sluggish.
Symptoms
The symptoms of hypothyroidism depend on how low your thyroid hormone is. These signs and symptoms can be vague and mimic other medical conditions. The symptoms tend to develop very slowly, sometimes even over several years. At first, the symptoms are barely noticeable, such as weight gain and fatigue. Many people think that the symptoms are the result of getting older. However, as your metabolism continues to slow down, you may experience more noticeable problems. The signs and symptoms include, but aren’t limited to:
- Cold intolerance
- Fatigue or tiredness
- Constipation
- Weight gain
- Dry skin
- Muscle and joint weakness, pain, and cramps
- Joint stiffness or swelling
- Puffy face
- Slowed movements, speech, and heart rate
- Depression
- Loss of libido
- Thinning hair
- Memory impairment
- Enlarged thyroid gland
The signs and symptoms of hypothyroidism can be different in infants. Hypothyroidism often occurs in middle-aged or older women, but it can also affect anyone, including infants. Infants born with a gland that doesn’t work properly or without a thyroid gland may experience few symptoms. The problem of hypothyroidism in babies usually include:
- Hoarse crying
- Difficulty breathing
- Protruding, large tongue
- Umbilical hernia
- Yellowing of the whites of the eyes and skin or jaundice.
As hypothyroidism progresses, infants often have trouble feeding and can fail to develop and grow normally. They may also have poor muscle tone, constipation, and excessive sleepiness. If hypothyroidism in infants isn’t treated, it can result in severe physical and mental development. Children and teens can also develop hypothyroidism. The symptoms are generally similar to adults, but children and teens may also experience:
- Delayed permanent teeth development
- Poor mental development
- Delayed puberty
- Poor growth, which results in a short figure.
If you have any symptoms of hypothyroidism, such as feeling tired for no reason, constipation, dry skin, or a hoarse voice, you should see a doctor as soon as possible.

Causes
- Hashimoto’s disease. The main cause of hypothyroidism is a condition called Hashimoto’s disease. It is an autoimmune disorder in which your body produces antibodies that attack your thyroid gland, resulting in inflammation and interfere with your thyroid gland’s ability to produce thyroid hormones. Viral infection can also cause thyroiditis.
- Thyroiditis. This condition occurs when your thyroid gland is inflamed. The inflammation causes the thyroid hormones to leak into your blood, which raises the overall levels and leads to hyperthyroidism (a condition in which a person produces too much thyroid hormone). After a couple of months, it can develop into hypothyroidism. Bacterial or viral infection, as well as an autoimmune condition or after pregnancy, can also cause thyroiditis.
- Over-response to treatment for hyperthyroidism. People with hyperthyroidism are usually treated with anti-thyroid medications or radioactive iodine. These treatments aim to get thyroid function back to normal. Sometimes, treating hyperthyroidism ends up reducing thyroid hormone production too much and results in permanent hypothyroidism.
- Radiation therapy. Radiation for cancers of the head and neck can affect your thyroid gland, leading to hypothyroidism.
- Thyroid surgery. Removing a large portion of your thyroid gland can halt hormone production and you will need to take thyroid hormone for life.
- Congenital disease. In the case of congenital hypothyroidism, your thyroid gland doesn’t function properly since birth. It can lead to physical and mental growth problems. However, early treatment can prevent any complications.
There are also other causes of hypothyroidism, such as medication, pituitary disorder, iodine deficiency or too little iodine in your diet, and pregnancy.
Risk factors
Hypothyroidism can affect anyone at any age, but some factors can increase your risk of developing the condition, including:
- Age. Hypothyroidism is more common among people older than 60.
- Gender. Women have a higher chance of developing hyperthyroidism.
- Race. Caucasians and Asians are a lot more prone to the condition.
- Genetic. Hypothyroidism can be hereditary. If you have a family history of thyroid disease, you are more likely to develop hypothyroidism.
- Certain medical conditions. Autoimmune disease, such as celiac disease or type 1 diabetes, makes you more prone to the condition.
- Certain medical treatments. Radiation therapy to your upper chest or neck as well as thyroid surgery can lead to hypothyroidism.
- Pregnancy. Having been pregnant or delivered a baby within the past six months increases your chance of developing the condition.
Diagnosis
To find out if you have hypothyroidism, your doctor usually reviews your medical history and will carry out a physical examination. Your doctor may advise you to take a blood test. The most common blood test is the thyroid-stimulating hormone (TSH) test, which detects the amount of TSH in your blood. If your TSH levels are above normal, you may have hypothyroidism. On the other hand, if the levels are below normal, you may have hyperthyroidism or hypothyroidism. To confirm the diagnosis and determine the cause, your doctor may perform additional tests, such as triiodothyronine, thyroxine, and thyroid autoantibody blood tests. Your doctor may also check your liver enzymes, prolactin, sodium, and cholesterol levels.
Treatment
The treatment of hypothyroidism focuses on supplementing the thyroid hormone. There is currently no cure for this condition, but there are treatments to help control it. The treatment normally involves taking daily hormone replacement tablets to raise your thyroxine levels. This tablet is called levothyroxine and is identical to the thyroxine hormone. You may need to take this tablet in the morning before eating every day. The dosage depends on your medical history, current TSH level, and the symptoms you experience. Your doctor will regularly monitor your blood to determine if the dosage of levothyroxine needs to be adjusted. At first, your doctor may check your TSH level after six to eight weeks, but then the blood levels are checked six months later.